What Is Myofascial Pain Syndrome a Guide to Relief
-
Myofascial pain syndrome, or MPS, is a tricky condition. It’s a chronic pain disorder centered around sensitive, tight knots in your muscles known as trigger points. These aren't just your average muscle aches; they cause a deep, persistent pain that has a peculiar habit of showing up in other parts of your body. This is called referred pain, and understanding it is the first real step toward finding relief that actually lasts.
Unraveling Myofascial Pain Syndrome
Think of a tiny, stubborn snag in a sweater. That one little pull can cause the fabric to bunch and pucker in a much larger area. A trigger point does something similar to your muscle tissue. It's a specific, irritable spot within the muscle and its surrounding connective tissue (the fascia) that creates tension and pain far beyond its own location.
This is why MPS can be so frustrating. The spot that hurts isn't always the source of the problem. You might have a persistent ache in your shoulder blade, but the real culprit could be a trigger point in a muscle in your neck. This is the whole concept of referred pain in a nutshell.
The Phenomenon of Referred Pain
Referred pain is the signature symptom of myofascial pain syndrome. A trigger point in one muscle can broadcast pain signals to a completely different, and often distant, part of the body. These patterns are surprisingly predictable once you know what to look for.
A classic example is a trigger point in the sternocleidomastoid muscle, which runs along the side of your neck. Knots here don't just cause neck pain; they can send pain signals up into your head, face, and jaw.
As you can see, that nagging headache behind your eye or that mysterious jaw ache might actually be coming from your neck. This is why just rubbing the sore spot often fails to bring relief—you have to find and treat the trigger point itself. It all starts with understanding what causes neck and shoulder tension to begin with.
If this sounds familiar, you're certainly not alone. Myofascial pain syndrome is incredibly common, affecting up to 85% of people at some point in their lives. In the U.S., it's estimated that nearly 44 million people deal with this condition. It's a widespread problem that deserves to be better understood.
The key takeaway is that MPS is a treatable, regional pain condition. Unlike widespread pain disorders, its symptoms originate from specific, localized trigger points within your muscles.
Myofascial Pain Syndrome vs General Muscle Soreness
It's easy to mistake MPS for the typical muscle soreness you feel after a tough workout. This quick comparison can help you tell the difference.
| Characteristic | Myofascial Pain Syndrome (MPS) | General Muscle Soreness (DOMS) |
|---|---|---|
| Cause | Trigger points from overuse, injury, stress, or poor posture. | Micro-tears in muscle fibers from strenuous, unfamiliar exercise. |
| Pain Type | Deep, aching, persistent pain. Often feels like a knot. | Diffuse, generalized ache across the entire muscle group. |
| Key Feature | Referred pain is common (pain felt in a different area). | Pain is localized to the muscles that were worked. |
| Duration | Can be chronic and persist for weeks or months if untreated. | Usually peaks 24-48 hours after exercise and resolves in a few days. |
| Response to Pressure | Pressing on a trigger point causes sharp, localized, and sometimes referred pain. | Gentle pressure or massage on the sore muscle generally feels good. |
Knowing whether you're dealing with a temporary ache or a specific trigger point is the first step in choosing the right path to relief.
Once you can identify these points, you can start using a much more targeted approach. Therapies that focus on the source—like trigger point massage or consistent heat application—are often the most effective. For instance, using a heated neck wrap can boost blood flow directly to a trigger point in your shoulder, helping those contracted muscle fibers finally relax and easing the referred pain you might be feeling in your head or down your arm. This gives you the power to manage your symptoms and get back to feeling like yourself.
The Science Behind Trigger Points
To really get a handle on myofascial pain syndrome, you have to understand what's happening on a microscopic level. The main culprit? Trigger points. Think of them as tiny, hyper-irritable knots of muscle fibers that have forgotten how to relax. It's like a small segment of a muscle gets a command to tighten up but then the 'off' switch breaks.
This constant contraction forms a palpable, tender nodule that wreaks havoc on the local neighborhood. It actually chokes off its own blood supply, which prevents oxygen and nutrients from getting in and stops metabolic waste from getting out.
This pile-up of waste products irritates the nearby nerve endings, creating that deep, nagging ache you feel when you press on a knot. The muscle itself becomes weaker and can't move as freely because it's being held hostage by these dysfunctional spots.
Demystifying Referred Pain
Now, here's where things get strange. The most confusing part of myofascial pain is referred pain. This is when a trigger point in one spot causes you to feel pain somewhere else entirely, often nowhere near the actual problem. It’s a bit like a short circuit in your body’s wiring—pressing a button in the kitchen makes a light flicker in the garage.
A classic example is a trigger point in the trapezius muscle, that large muscle spanning your upper back and shoulders. When it gets knotted up, it often sends pain shooting up the side of your neck and into your temple, creating a textbook tension headache. You could rub your temples all day long, but the relief won't last because the source of the problem is still active in your shoulder.
This simple map shows how that frustrating chain reaction works, from the hidden trigger point to the pain you actually feel.
As you can see, a single muscle knot can cast a wide net of discomfort. This is precisely why it’s so important to treat the source, not just chase the symptoms.
Why Targeted Therapies Work
Knowing how trigger points operate is half the battle. Once you can pinpoint where the pain is really coming from, you can use treatments that actually make a difference. Two of the most effective and easy-to-use therapies are heat and massage.
Heat Therapy
Applying warmth to a trigger point works wonders. The heat boosts circulation, which accomplishes two key things:
- It delivers a fresh supply of oxygen-rich blood to the starved muscle fibers.
- It helps flush out all those built-up waste products that are aggravating your nerves.
For example, draping a microwavable heat pack over your shoulders for 15-20 minutes allows gentle, deep-penetrating warmth to reach the trapezius muscle. This encourages those tight, stuck fibers to finally let go, which can dissolve the knot and ease that referred headache. The benefit of this is clear: you get profound relief that lasts, rather than just masking the symptoms for an hour or two.
Massage Therapy
Massage, on the other hand, applies direct, sustained pressure to the trigger point. This manual pressure physically breaks up the knot and encourages the contracted fibers to release. It also gets the blood flowing, much like heat does. You can even do this yourself using your fingers or a massage tool.
Say you have a trigger point in your calf that’s sending pain into the arch of your foot. You could sit down and use your thumb to apply gentle, firm pressure to that tender spot for 30-60 seconds. Combining this with heat beforehand can make the muscle much more receptive to the massage. A key benefit here is that you're taking an active role in your own recovery, gaining the power to address pain the moment it starts, without having to wait for an appointment.
By directly targeting the trigger point with these methods, you're not just masking the pain—you're addressing the root cause for more meaningful, lasting relief. For more ideas, take a look at our guide to natural remedies for muscle soreness.
What Causes Myofascial Pain Syndrome?
To get a handle on myofascial pain, you first need to understand where it comes from. It rarely just shows up one day for no reason. Instead, it’s usually the end result of very specific stresses piling up on your muscles over time.
Think of these triggers as falling into two main buckets. On one hand, you have direct muscle strain. On the other, you have bigger-picture issues within your body that make your muscles more vulnerable in the first place.
Acute Injuries and Repetitive Strain
Direct muscle overload is, by far, one of the most common culprits. This can happen from a sudden, one-off event, but more often it’s the small, repetitive movements we do every single day that cause the most trouble.
Here are some of the usual suspects:
- Sudden Trauma: A car accident causing whiplash, a bad fall, or a sports injury can instantly damage muscle fibers, setting the stage for trigger points to form as the muscle tries to protect itself.
- Poor Posture: This is a big one. Spending hours slumped over a desk, slouching on the sofa, or staring down at your phone puts a relentless, low-grade strain on the muscles in your neck, shoulders, and back.
- Repetitive Motions: Any job or hobby that involves doing the same thing over and over can wear out specific muscles. Think about typing, using a computer mouse for hours, lifting boxes, or even gardening.
Learning how to prevent running injuries and stay strong and healthy offers a great blueprint for avoiding this kind of overuse, and the core principles apply to almost any activity, not just running.
Systemic and Lifestyle Risk Factors
While direct strain is a huge piece of the puzzle, your overall health and daily habits are just as important. Certain conditions and lifestyle choices can create an internal environment that makes it much easier for trigger points to develop and stick around.
These sneaky factors often include:
- Psychological Stress: When you’re stressed or anxious, what’s the first thing your body does? It tenses up. If that tension becomes chronic, it chokes off blood flow to your muscles and can easily create painful knots.
- Poor Sleep: Our muscles do their most important repair work while we're in deep sleep. If you're not getting enough quality rest, you rob them of this critical recovery time, leaving them tired and much more susceptible to irritation.
- Nutritional Gaps: Your muscles need the right fuel to function properly. Being low in key vitamins and minerals—like Vitamin D, iron, or magnesium—can directly impair muscle health and contribute to pain.
A Real-World Example: Imagine 'David the Desk Worker.' He spends eight hours a day at his computer, and his head naturally drifts forward, putting a constant, nagging strain on his neck muscles (repetitive strain). On top of that, tight deadlines keep his shoulders hiked up toward his ears all day (psychological stress). This combination is a perfect storm for developing trigger points in his upper back and shoulders, which eventually lead to stubborn tension headaches. Understanding this connection is incredibly helpful because it gives David specific, actionable areas to focus on for relief, such as improving his desk ergonomics and incorporating relaxation techniques.
The medical world's understanding of MPS has grown exponentially over the last few decades. Between 1956 and 2022, a total of 1,099 research papers on the topic were published across 57 countries. The United States has led this effort with 270 publications, which is 24.57% of the total research.
This surge in knowledge helps explain why this condition, found in up to 30% of patients visiting primary care for pain, is finally getting the attention it deserves.
How Professionals Diagnose and Treat MPS
Finding your way to relief from myofascial pain starts with a solid diagnosis. Because there isn't a single blood test or X-ray that can pinpoint MPS, the process relies on a skilled, hands-on clinical evaluation. This step is so important—it validates what you're feeling and lays the groundwork for a treatment plan that actually works.
A practitioner who knows their stuff, like a physical therapist or a pain management specialist, will start with a thorough physical exam. They’ll use palpation—a fancy word for feeling with their fingers—to carefully search for the classic signs of MPS. What they're looking for are those tight, rope-like bands of muscle and the angry little knots, the trigger points, hiding within them.
When a trigger point is found and pressed, it usually reproduces your exact pain. You might feel a local muscle twitch and that familiar ache radiating to another part of your body. For many people, this moment is a huge relief; it finally gives a name and a physical cause to what's often been a confusing and frustrating experience.

Hands-On Therapies for Lasting Relief
Once MPS is diagnosed, a whole world of effective, hands-on treatments opens up. These therapies are all about manually releasing those contracted muscle knots, getting things moving properly again, and breaking the cycle of pain. Working closely with your healthcare provider is the best way to figure out the right combination for you.
A physical therapist, for instance, can build a personalized program of stretches and strengthening exercises. This approach does two things: it deactivates the trigger points you have now and, just as importantly, it corrects the muscle imbalances or postural habits that caused them, helping to prevent future flare-ups.
This kind of targeted therapy is critical, especially when pain is complex. One study of head and neck cancer patients found that a staggering 68.3% also had Myofascial Pain Syndrome. This really underscores how MPS can get tangled up with other serious health conditions, and it shows why specific physical therapies are so vital for managing chronic pain.
Specialized Treatments and At-Home Support
Beyond foundational physical therapy, a few other treatments are incredibly effective for getting at those really stubborn trigger points and providing deeper relief.
- Specialized Massage Therapy: This isn't your typical spa massage. A therapist trained in trigger point therapy uses deep, sustained pressure right on the knots to convince them to release. The benefit is profound: this targeted approach helps improve blood flow and melt away tension at the source, offering much longer-lasting relief than a general relaxation massage.
- Dry Needling: A practitioner inserts very thin, sterile needles directly into your trigger points. This isn't acupuncture; instead of focusing on energy meridians, dry needling is all about physically releasing the tight muscle bands and kick-starting a healing response.
- Trigger Point Injections: For knots that just won't give up, a doctor might inject a local anesthetic or even just a saline solution into the trigger point. This can help flush out inflammatory substances and mechanically break up the contracted fibers.
The goal of professional treatment is to deactivate the trigger point. But long-term success depends on integrating what you learn into your daily life. The most effective plans combine professional guidance with consistent self-care.
This is where you can take control, especially with something as simple as heat therapy. Applying a microwavable heat pack to a sore muscle before you stretch can make the tissue much more flexible and ready to release. For example, warming your lower back for 15 minutes before doing gentle stretches can dramatically reduce stiffness and pain. The benefit here is that the work you do in physical therapy becomes much more effective, helping you see progress faster. For more ideas, you can check out our guide on other back treatments you may not have tried.
By teaming up with a professional and embracing these supportive therapies at home, you can create a powerful plan that not only tackles your immediate pain but also empowers you to manage your symptoms for the long haul.
Empowering Self-Care for Daily Pain Relief
While professional treatments lay the foundation for recovery, the real power to manage myofascial pain syndrome is in your daily habits. This is where you take control.
Building a solid at-home toolkit, with cornerstone therapies like heat and massage, can provide immediate, drug-free relief. More importantly, it empowers you to manage your symptoms effectively day-to-day.
These self-care strategies aren't just about temporary comfort; they're about actively participating in your own healing. By learning to listen to your body and respond with targeted care, you can break the pain cycle and stop minor stiffness from escalating into a full-blown flare-up.
The Transformative Power of Heat Therapy
Heat therapy is one of the best tools for tackling the stubborn knots of MPS. Think of a trigger point as a muscle that's starved for oxygen and choked by its own waste products. Applying warmth is like opening a superhighway for healing.
The benefit of using heat is that it works naturally with your body. It boosts circulation, allowing fresh, oxygen-rich blood to flood the area. This influx of blood delivers vital nutrients and helps flush out the pain-causing metabolic waste trapped in the contracted muscle fibers. This whole process helps the muscle relax on a chemical level, soothing irritated nerves and melting away the tension that holds the knot in place.
A Step-by-Step Guide to Using a Heat Pack
Using a microwavable heat pack is a simple yet powerful way to apply this therapy. Let’s walk through how to do it for that common trigger point in your trapezius muscle—the one that often sends pain right up into your head.
- Heat Your Pack: Follow the instructions to warm your pack safely in the microwave. You're aiming for a deep, soothing warmth, not scorching heat.
- Get Comfortable: Find a quiet, comfortable place to sit where you can relax your neck and shoulders without any strain.
- Apply and Relax: Drape the heated wrap over your shoulders, making sure it has good contact with the muscles on both sides of your neck and upper back.
- Breathe and Let Go: Close your eyes and take slow, deep breaths. Allow the gentle, sustained warmth to penetrate the trapezius muscles for 15-20 minutes.
- Feel the Change: As the muscles absorb the heat, you should feel the tension start to dissolve. This simple act can ease not only the local knot but also that referred headache behind your eyes.
Unlocking Knots with Self-Massage
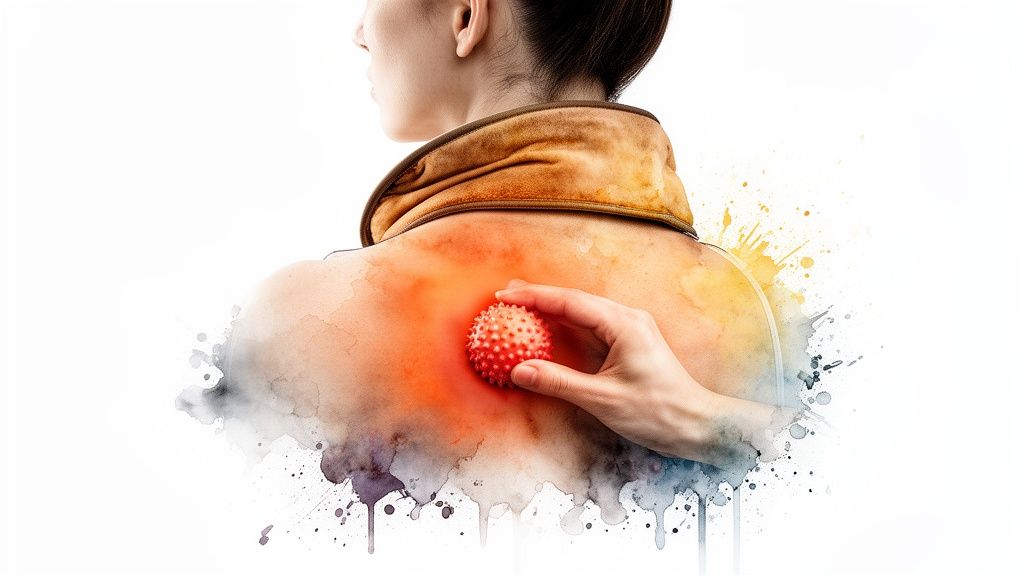
Once your muscles are warm and more pliable, it’s the perfect time for some gentle self-massage. This technique applies direct, sustained pressure to the trigger point, manually encouraging the knotted fibers to finally let go. You don't need to be a professional masseuse; you just need to be patient and gentle.
The primary benefit of self-massage is empowerment. Using your own hands or a simple tool like a massage ball gives you total control over the pressure, allowing you to target the exact source of your pain the moment it starts.
The combination of heat followed by massage is a classic one-two punch for myofascial pain. Heat prepares the muscle by making it more flexible, and massage delivers the targeted pressure needed to release the knot. This is incredibly helpful because it makes your self-treatment sessions more effective and provides faster, more significant relief.
How to Perform Simple Self-Massage
Let’s say you have a nagging trigger point in your upper back, right beside your shoulder blade—a notoriously hard-to-reach spot.
- Using a Massage Ball: Place a massage ball (a tennis or lacrosse ball works, too) between your back and a wall. Lean into it, rolling gently until you find that tender, knotted spot. Hold steady pressure on the trigger point for 30-60 seconds while breathing deeply. Be careful not to press so hard that you cause sharp pain.
- Using Your Hands: For more accessible areas like your neck or calves, use your fingertips or thumb to apply firm, sustained pressure directly to the knot. You can also gently knead the area in small circles to further encourage the release.
These at-home therapies give you the ability to address pain the moment it starts. And while you're building your toolkit, it’s worth noting that among the various complementary approaches, exploring the extensive red light therapy uses for pain relief can also offer promising avenues for managing MPS symptoms.
By consistently incorporating these simple, actionable strategies into your routine, you build resilience and reclaim control from chronic pain.
A Sample Daily Routine for Managing Myofascial Pain
Alright, we've covered the science behind myofascial pain, but what does managing it actually look like day-to-day? Theory is one thing; a practical plan is where the real relief begins.
Let's walk through a day in the life of 'David the Desk Worker' to see how these concepts come together. This isn't about a massive, time-consuming overhaul. It's about weaving small, smart habits into your existing schedule to make a big impact.
Starting the Day Right
David used to be a "snooze button and scramble" kind of guy, starting his day already feeling tight and stiff. His new approach is all about gently waking up his body and setting a better tone for the day.
- 7:00 AM - Gentle Movement (10 minutes): Before his feet even hit the floor, David spends about ten minutes on some simple, in-bed stretches. Think easy neck rotations, shoulder rolls, and gentle spinal twists. It’s a simple way to shake off that overnight stiffness and get the blood moving.
- 7:15 AM - Morning Heat Therapy (15 minutes): While the coffee is brewing, David pops his microwavable neck wrap in for a minute. He drapes it over his shoulders and neck while he catches up on the news. This is so helpful because the deep, soothing heat melts away any lingering tension, preventing morning stiffness from dictating the rest of his day.
Navigating the Workday
Like for so many people, David's desk job was the primary source of his pain. Instead of just gritting his teeth through it, he now has a strategy to keep those trigger points from flaring up.
He’s added a supportive lumbar pillow to his office chair, a small change that makes a huge difference in preventing the chronic, low-grade muscle strain in his lower back.
David now lives by the 50/10 rule. He works for 50 minutes, then takes a mandatory 10-minute micro-break. He doesn't just scroll on his phone—he gets up, stretches his arms overhead, does a lap around the office, and resets his posture. This simple rhythm is beneficial because it prevents muscle fatigue and stiffness from building up throughout the day.
Winding Down for a Better Night's Sleep
The end of the day is your best chance to release any tension you've accumulated. A solid evening routine helps your muscles recover and sets you up for truly restful sleep.
- 6:30 PM - Targeted Massage (10 minutes): After work, while unwinding with a podcast, David grabs a massage ball. He stands against a wall and uses it to apply gentle, sustained pressure directly on the trigger points in his upper back and shoulders. This is a great way to work out the knots that built up during the day.
- 9:30 PM - Soothing Heat Session (15 minutes): Just before heading to bed, he has one last session with his heating pad, this time placing it on his lower back. The warmth not only relaxes his muscles but also calms his nervous system, making it easier to fall asleep and reducing the odds of waking up in pain.
By layering these small habits—heat, massage, movement, and better posture—David has taken back control from his chronic pain. His simple, consistent routine doesn't just manage his myofascial pain syndrome; it helps prevent flare-ups so he can get back to doing what he loves.
Still Have Questions About Myofascial Pain?
If you're dealing with chronic muscle pain, you've probably got a lot of questions. That’s completely normal. Let's clear up some of the most common points of confusion about myofascial pain syndrome to help you feel more confident on your path to feeling better.
Can Myofascial Pain Syndrome Ever Go Away Completely?
For many people, the answer is a resounding yes. MPS can often be resolved, especially if it’s tied to a clear, fixable cause—think a past injury that healed improperly or even just a bad desk setup at work.
With the right mix of professional treatment and dedicated self-care, it’s entirely possible to deactivate those trigger points and get rid of the pain for good. If your MPS is linked to another chronic condition, the goal might shift from a complete "cure" to smart, effective management. Learning what triggers your flare-ups and using simple at-home strategies can give you the power to control your symptoms and stay active.
What Is the Difference Between Myofascial Pain and Fibromyalgia?
This is probably one of the most common questions we hear, and it's a great one. While both cause chronic muscle pain, they are very different conditions at their core. Myofascial pain syndrome is what we call a regional pain disorder. The pain comes from very specific, irritable knots—trigger points—in a single muscle or a group of muscles, and it tends to refer pain in predictable patterns.
Fibromyalgia, on the other hand, is a widespread pain condition. It involves tenderness all over the body, in multiple quadrants, not just isolated spots. Fibromyalgia also brings a host of other symptoms like deep fatigue, serious sleep problems, and cognitive difficulties often called "fibro fog." To make things more complicated, it's absolutely possible to have both conditions at the same time.
The real difference comes down to scope. Think of MPS as localized pain stemming from trigger points, while fibromyalgia is generalized, body-wide pain that comes with a wider range of systemic issues.
Is It Better to Use Heat or Cold for Myofascial Pain?
When you’re dealing with the deep, chronic tension and knotted-up muscles of myofascial pain, heat is almost always the way to go. Heat therapy does two fantastic things: it boosts blood flow to those tight, starved muscle fibers, helping them relax, and it calms the irritated nerves, which dials down the pain signals.
Think about draping a warm neck wrap over your shoulders. That deep, comforting warmth coaxes those tight knots to finally let go. Cold therapy, like an ice pack, is really best for fresh, acute injuries where there’s obvious swelling—like a sprained ankle. In fact, putting ice on a chronic trigger point can sometimes make the muscle clench up even more, which is the last thing you want.
Ready to feel the difference that targeted heat therapy can make? Check out the full line of American-made, clinic-trusted heat wraps at SunnyBay. Find the perfect wrap for your neck, back, or shoulder pain and start living more comfortably. Visit the SunnyBay website to learn more.



